What Causes a Sore Vagina?
Steph Coelho is a freelance health writer, web producer, and editor based in Montreal. She specializes in covering general wellness and chronic illness.
Learn about our editorial processUpdated on March 16, 2022Medically reviewedVerywell Health articles are reviewed by board-certified physicians and healthcare professionals. Medical Reviewers confirm the content is thorough and accurate, reflecting the latest evidence-based research. Content is reviewed before publication and upon substantial updates. Learn more.byMonique Rainford, MD Medically reviewed byMonique Rainford, MDMonique Rainford, MD, is board-certified in obstetrics-gynecology, and currently serves as an Assistant Clinical Professor at Yale Medicine. She is the former chief of obstetrics-gynecology at Yale Health.
Learn about our Medical Review BoardTable of ContentsView AllTable of ContentsThere are a lot of possible reasons why you may be experiencing pain or soreness in and around your vagina. Some, like irritation or menopause, may be obvious. Others, like a sexually transmitted infection or a cyst, less so.
What people call "vagina pain" may indeed involve the vagina, the inside part that connects to the womb or uterus. But it may also involve the vulva, the outer part of the genitals.
This article explores some of the causes of a vulvar or vaginal pain and soreness. It also explains how these problems are diagnosed and treated.
Causes
Vaginal pain can have many different causes. Some are serious, while others go away on their own or respond to simple treatments.
Yeast Infection
A yeast infection is caused by a fungus. It can cause pain and itching around the vulva and vaginal opening. Other symptoms include:
Some people are more prone to yeast infections. This includes people who:
In some cases, hygiene habits can raise your risk (for example, not quickly changing out of sweaty workout clothes).
How to Get Rid of a Yeast InfectionBacterial Vaginosis (BV)
Bacterial vaginosis is an infection that happens when too much of a bacteria grows in your vagina. Not everyone has symptoms.
If you do, you might notice:
Your risk of getting BV is higher if you:
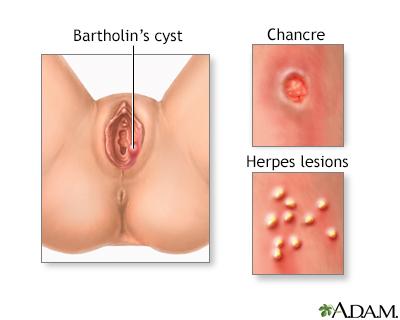
Treatment Options for Bacterial VaginosisSexually Transmitted Infections
Sexually transmitted infections (STIs) can also cause vaginal/vulvar pain, as well as itching and burning.
Some examples include:
If you think you could have an STI, talk to your healthcare provider. You and your partner should both be tested to reduce the risk of passing it on or having complications.
Why You Might Not Realize You Have an STDUrinary Tract Infection
Urinary tract infections (UTIs) are very common. UTIs happen when bacteria enter the urinary tract.
Symptoms include:
A UTI can make it painful to have sex.
Getting Rid of a UTIIrritation or Allergy
Irritation and allergies can cause soreness. You may have a reaction to:
Shaving or waxing the area can also cause discomfort, especially when the hair grows back. This pain is usually temporary.
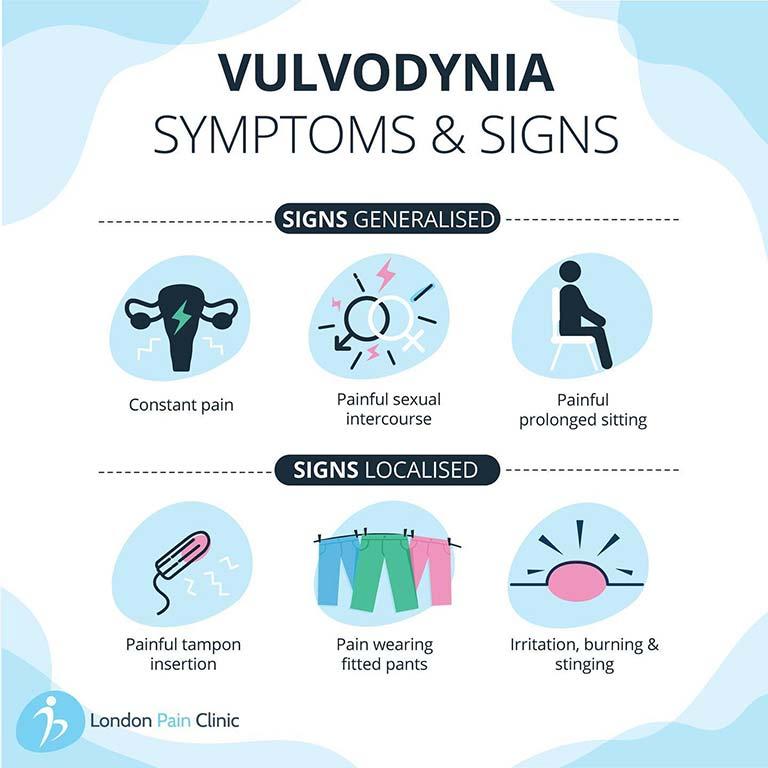
Vulvodynia
Vulvodynia is vulvar pain that lasts more than three months. You may also notice:
Genetics, hormones, or nerve damage may raise you risk. Vulvodynia can also happen after medical procedures such as surgery or chemotherapy.
Bartholin’s Cyst
A Bartholin’s cyst occurs when the Bartholin glands on the labia, the skin folds around the vaginal opening, become blocked.
A cyst that’s not infected may show up as a painless lump. These often resolve on their own.
If a Bartholin cyst becomes infected, it might swell up, be painful, and make it harder to walk or sit comfortably. This may require treatment.
Endometriosis
Endometriosis is when the lining of the uterus (womb) builds up on the outside of the organ. Not everyone has the same symptoms.
Some common symptoms of endometriosis include:
Pelvic Floor Problems
Pelvic floor dysfunction is a health condition where the muscles and tendons in your pelvic area weaken. It can cause vaginal pain, especially during sex.
If you have pelvic floor dysfunction, you may leak urine or have trouble controlling bowel movements.
These problems can be caused by:
Menopause
Vaginal pain can also occur because of hormonal changes during menopause. The vagina may become drier. Skin can become thin and easy to tear. These changes can make sex painful.
Other symptoms include:
There is also an increased risk of infection, which can itself lead to vaginal pain.
Vigorous Sex
The tissue in and around the vagina can tear or bruise during rough sex, leading to soreness. Sex can also lead to chafing around the vulva.
These symptoms are more likely if the skin is thin, dry, scarred, or affected by a health condition such as eczema or psoriasis, although all vaginal skin is delicate.
If you think you may have an injury inside your vagina, seek medical care. In rare cases, internal bleeding can be life-threatening.
If you have been sexually assaulted, reach out for help as soon as you are safe. One way to get help is to call the National Sexual Assault (RAINN) Hotline at 800-656-HOPE (4673). You can also speak to a healthcare professional you trust.
Vaginismus
Vaginismus is a condition where vaginal muscles spasm. It can make it difficult to have sex. It can also cause pain.
People may develop vaginismus in response to trauma. It can happen because you're nervous about having sex. But it can also occur during menopause or after childbirth.
Trauma
If you've just had a baby, your vagina will be sore for a period of weeks afterward. Sometimes pain from childbirth lasts even longer.
Injuries from straddle accidents, vehicle accidents, sexual assault, and female genital cutting can also cause long-term pain.
When to See a Healthcare Provider
If your symptoms are bothering you and don’t go away, see a healthcare professional.
It's especially important to seek medical care if you have vaginal pain or soreness and are pregnant, in menopause, or have a new sex partner.
Seek immediate medical attention if you have been sexually assaulted. Do not clean yourself of change your clothes ahead of your visit.
Other signs that you need to see a doctor:
Diagnosis
It can take time to find out exactly what is behind your pain. To identify the cause, a healthcare professional may:
Treatment
Treatment will depend on the exact cause of your soreness or pain. In some cases, changing your routines may be all that is needed. In others, medical intervention may be necessary.
Home Remedies and Lifestyle
For example, it may help to:
Medications
Conditions like STIs need to be treated. They won’t go away on their own and can cause serious consequences if left untreated.
If the pain is from something like endometriosis, a healthcare provider can help you manage symptoms with medications, including:
Physical Therapy
Your therapist may work with you to build your pelvic floor muscles.
Some people learn to relax vaginal muscles using dilators, which are tapered wand-like tools that come in various sizes.
Psychotherapy
Cognitive behavioral therapy can teach you strategies to relax tense muscles or cope with anxiety, trauma, or pain.
Surgery
If the pain does not go away with other treatments, you may need surgery. For example, if you have an infected Bartholin's cyst, it may need to be drained.
In some cases, surgery to remove scar tissue helps with endometriosis symptoms. A hysterectomy—removal of the uterus—is another option for endometriosis.
Prevention
To protect your vulva and vagina, you can:
Summary
Pain in or around your vagina can have many possible causes. Infection, injury, health conditions, menopause, childbirth, pelvic floor problems, and allergies can all make the vulva or vagina sore.
Don't ignore vaginal pain. Most of the time, it will go away on its own or with self-care. But some types can be serious. Medication, physical therapy, and even surgery may be needed to restore your health.
A Word From Verywell
Some healthcare providers minimize women's concerns about pain. This is especially true when patients are women of color, trans women, women with low incomes, and women with a history of substance use disorders.
When you're seeking care for vaginal pain—or anything else—you need a healthcare provider who takes your symptoms seriously. If you don't feel heard and respected, look for another provider.
Was this page helpful?Thanks for your feedback!Sign up for our Health Tip of the Day newsletter, and receive daily tips that will help you live your healthiest life.
You're in!Thank you, {{form.email}}, for signing up.
There was an error. Please try again.